Stevens-Johnson Syndrome/Toxic Epidermal Necrolysis
Background
- Stevens-Johnson Syndrome (SJS) and Toxic Epidermal Necrolysis (TEN) are severe skin reactions (usually to medications) that constitute dermatologic emergencies
- Common culprit medications: antibiotics, anti-epileptic drugs, NSAIDs
- SJS and TEN are the along the same disease spectrum, TEN is just clinically more severe and widespread
- The extent of epidermal detachment is <10% total body surface area (tBSA) in SJS and >30% tBSA in TEN
- This is a rare disease (1 case per million per year), but is more common in patients with HIV/autoimmune disorders/immunosuppression and the elderly (likely because of this population's increased use of medications).
- Certain genetic markers are associated, especially HLA markers.
- In bone marrow transplant patients, TEN can be indistinguishable from acute graft vs host disease
- The mechanism is thought to be the host's inability to metabolize the offending drug, which results in toxic metabolite buildup, which then activates T cells and keratinocyte apoptosis.
Presentation
- Typically occurs 4 days to 4 weeks after the drug exposure
- Patient initially has nonspecific viral symptoms, then develops a macular rash that is painful, pruritic, and morbilliform (macular/red/sometimes confluent like measles) on the face and trunk.
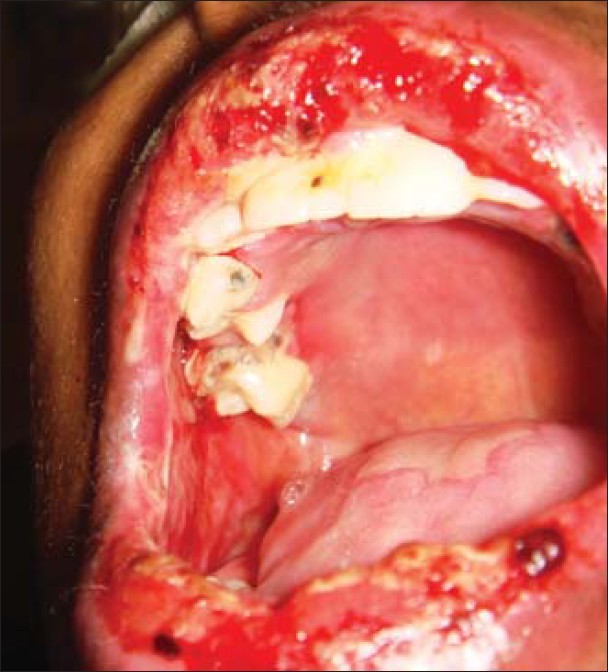
- Lesions progress with sheets of epidermal detachment from dermis (Nikolsky's sign- separation of the skin with slight pressure- can be seen).
- Mucosal involvement is common
- Rarely, internal organs, particularly in the respiratory/GI tracts can undergo necrosis, causing symptoms such as respiratory distress and diarrhea
- DDx should include: Staphylococcal scalded skin syndrome (SSSS)/AKA Ritter diseases, Graft vs host disease (GVHD), bullous pemphigoid, pemphigus, acute generalized exanthematous pustulosis (also usually a febrile drug reaction occuring ~5 days after drug exposure, characterized by numerous small pustules but no mucosal involvement)
Management
- Withdraw causative drugs
- Supportive care
- Wound care, infection control, fluid and electrolyte replacement
- Essentially waiting for the skin to heal on its own, similar to in burn patients
- Re-epithelialization occurs within a few days to weeks
- Some studies show improvement with IVIg but this is not standard of care
- Blocks TNF-alpha-induced apoptosis,
- Avoid this in renal failure
- Steroids have been used in the past but there are no good trials that support their use and they have been demonstrated to be more harmful in advanced cases
- Avoid silver-sulfadiazine in wound care since sulfas can induce SJS/TEN
Prognosis
- Overall SJS has a 1-5% mortality; TEN has a 25-35% mortality, mostly due to infection of non-intact skin
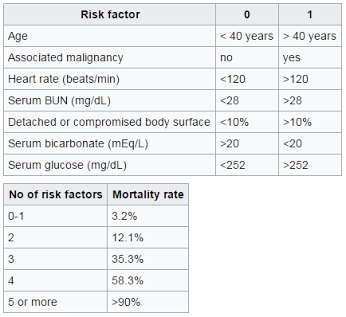
- The SCORTEN scale can be used in TEN, regular burns, or other cutaneous drug reactions to assess prognosis
- Risk factors include age, associated malignancy, heart rate, BUN, %tBSA involved, bicarbonate level, glucose level