Capnography use in the ED
What is it?
Waveform Capnography is a continuous, noninvasive measurement of end-tidal Co2 or ETCo2 (also called PetCo2). Capnography uses a simple sensor to monitor the amount of expired Co2, it also shows -in waveform- the amount inhaled and exhaled Co2. This waveform is usually rectangular in shape and displays the patient's ETCo2, respiratory rate, and tidal volume. It offers both quantitative and qualitative measures. Being able to continuously monitor these values may help the physician determine the patient's condition throughout his/her care or can help provide a potential differential diagnosis by allowing to monitor pulmonary ventilation directly as well as indirectly monitoring metabolism. Two sensors can be used to measure capnography, a nasal prong or an adapter that can be combined with a BVM or an advanced airway. It can either be mainstream or sidestream capnography where the main differences are; mainstream monitoring is direct and in real-time and in sidestream, the monitoring is indirect and delayed because air is diverted at a T-piece to an external sensor. This delay is simply because the T-junction and length of the tubing create dead space between it and the sensor itself which causes a delay. Capnography is used extensively in the field by paramedics however, it’s also very helpful in a hospital setting as well.
How it works?
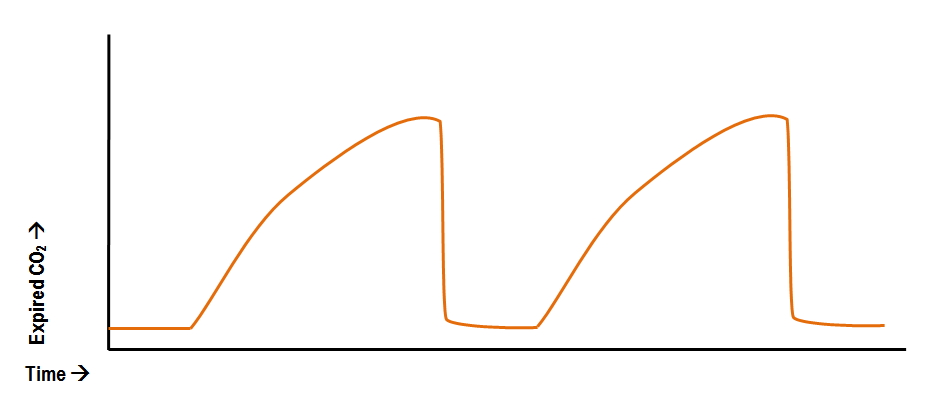
Briefly, cellular metabolism produces carbon dioxide, while the lungs work to eliminate it from the body. The balance between production and elimination of Co2 can be noted as the rise and fall (respectively) of the waveform. Looking at the graph, the x-axis represents the partial pressure in mmHg while the y-axis displays time in seconds. Referring to the media attached (Basic Waveform), the beginning of the expiration can be noted by the flat line also known as the baseline (Phase I). As the patient breathes out, the graph curves upwards (Phase II) which displays the transition from dead space air flow to alveolar air flow. Eventually, the curve hits a plateau (Phase III) which represents the partial pressure of Co2 exchanged at the alveoli, this value denotes the end-tidal Co2. Following the plateau, the patient breathes in air and this can be seen by the downward deflection (Phase IV) which indicates a decrease of carbon dioxide levels and an increase in fresh air flow. Values are calculated in mmHg (millimeters of mercury) with a normal value range of 35 - 45 mmHg and may fluctuate above or below these norms depending on the patient's condition. For example, a decrease in perfusion will lead to a decrease in ETCo2 by limiting the amount of Co2 traveling to the lungs, this can be seen on the capnograph by a waveform below 35 mmHg. When the values are above 45 mmHg we say that the patient is in hypercapnia (also known as hypercarbia) and when the patient is below we say that the patient is in hypocapnia (hypocarbia)
Usefulness
Capnography is used in many situations both in the ED and Prehospital care;
-
Confirmation of tracheal intubation
-
Accessing tracheal tube placement and tracheostomy potency and placement
-
Monitoring adequate ventilatory support
-
During percutaneous tracheostomy placement
-
Monitoring patients with increased ICP
-
Monitor patient’s response to treatments
-
Estimation cardiac output and metabolism
-
Multiple uses in cardiac arrest
As you can see, the multitude of situations where capnography can be used in the ED is quite extensive. Therefore, we’ll visit each point one by one and elaborate on their uses.
Confirmation of tracheal intubation
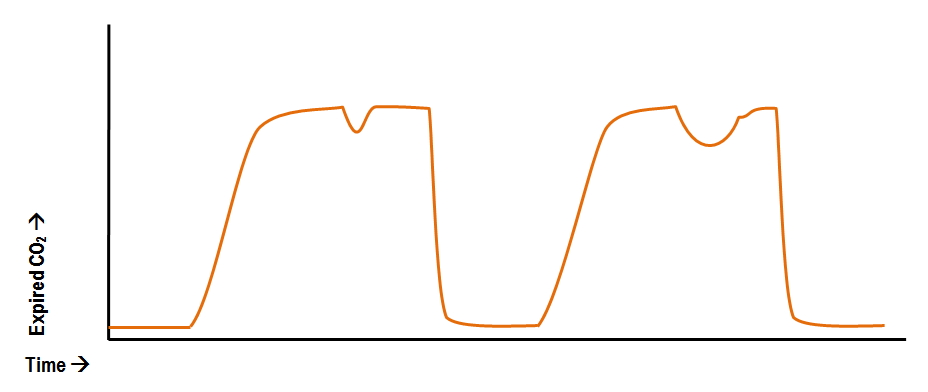
Capnography is recommended during intubation, it allows the physician to verify adequate ventilation and FiO2 prior to the intubation as well as tube placement after the intubation. Once the patient reaches an adequate ventilatory status including saturation, respiratory rate, and capnography waveform, the patient is then intubated. This prior monitoring confirms that the patient is adequately ventilated and that the intubation will not deteriorate his/her condition -during the intubation- to the point of cardiac or respiratory arrest. Once the tube is placed, the capnograph should indicate adequate values between 35 - 45 mmHg as well as a good waveform with all four phases. In the case of esophageal tube placement, the typical waveform is a straight flat line with no values. In rare cases, the stomach may contain some traces of Co2 but is seen as short decreasing waveforms with a duration of 1-6 waveforms before showing a flat line. If the physician inadvertently and unintentionally performs endobronchial intubation, it can be seen as a notch during the expiratory phase indicating that more air is coming for one lung then is slowly mixed with other lung’s air. (see attached media) Although other methods are available in verify placement such as auscultation, chest movement and fogging of the tube, however, capnography offers a more reliable and consistent data.
Accessing tracheal tube placement and tracheostomy potency
Capnography can also be used as a method for continuous appreciation of a patient’s ventilatory status while intubated or in post tracheostomy. Any changes in the waveform or any other values should prompt the physician to respond, assess and correct the situation. In an intubated patient, capnography can display if the patient is trying to breathe by him/herself. This can be identified because, during their feeble inspiratory effort, fresh air can get sucked in and is displayed on the waveform as a depression during the plateau phase. This is called a curare cleft and may prompt the physician to reevaluate the patient. (see Curare Cleft attached media)
Monitoring adequate ventilatory support
The use of capnography on a patient with ventilatory support goes beyond intubated patients or patients with a tracheostomy. It can be used to monitor any patients that are under mechanical ventilation and assess their adequacy as well as the ventilatory status of any patients that require monitoring. Hypoventilation can be seen as hypercapnia (High ETCo2) while hyperventilation can be seen as hypocapnia (Low ETCo2). When the patient is hypoventilating a greater amount of Co2 is expired therefore it shows a rise in ETCo2 and vice versa. This allows the physician to make the necessary adjustments. This type of monitoring extends beyond hyper and hypoventilation and can be used to determine bronchospasms, obstructions, emphysema, hypothermia and poor lung compliance all according to the waveform produced by the capnograph.
During percutaneous tracheostomy placement
Using the same purpose of ETT placement, capnography can be used during percutaneous tracheostomy by verifying tracheostomy placement at the end of the procedure
Monitoring patients with increased ICP
Capnography can also help the physician monitor patients with increased intracranial pressure and anticipate the rise and fall of pressure. This can be done simply because an increase in ETCo2 is directly proportional to an increase in cerebral blood flow which increases intracranial pressure. Inversely, a low ETCo2 causes vasoconstriction of cerebral blood flow which decreases intracranial pressure. Therefore, it can be used as a continuous monitoring tool during ICP management.
Monitor patient’s response to treatments
Capnography has been used extensively to assess a patient's response to treatment especially bronchodilators in the case of bronchospasms. Bronchospasms can be seen on the capnograph by an exaggerated up-sloping during phase II which is associated to slow expiration. Therefore, a physician can administer a bronchodilator and re-evaluate the capnography waveform to check if the up-sloping is still present or it’s decreasing. By identifying this slow up-slope, diagnosing bronchospasms with capnography can also be done.
Estimation cardiac output and metabolism
Since excretion of Co2 depends on pulmonary blood flow, the physician can use capnography as a mean to estimate the cardiac output. Like the previous example, a decrease in perfusion will result in a decrease of ETCo2 (Assuming ventilations are constant). Capnography can also indirectly identify metabolism distress such as sepsis or acidosis. The link between ETCo2 and metabolism is a quite a simple one. If blood pH decreases, the metabolic and respiratory buffer will increase in order to maintain equilibrium. Therefore, respiratory rate will increase and this will lead to hypocapnia (Low Co2 levels). Same physiological response occurs in the case of sepsis where lactate levels increase due to organ hypoperfusion which, in turn, increases the buffer system activity. In conclusion, an increase in metabolism results in an increase of respiratory rate, leading to a decrease in Co2. This relation can also be seen in the opposite scenario, where alkalosis causes hypercapnia.
Multiple uses in cardiac arrest
-
Confirmation of advanced airway placement
-
Monitoring of ventilation rate and avoiding hyperventilation
-
Assessing adequate compressions
-
Identifying ROSC (Return of spontaneous circulation)
These are the multiple uses of capnography during cardiopulmonary resuscitation. The confirmation of advanced airway placement is done the same way as the prior discusses ETT placement verification. Once intubated, the physician can monitor the ventilatory rate and assure that the patient is not hyper or hypoventilated. During compressions, the physician can assess proper compressions by verifying that the ETCo2 is > 15 mmHg which consequently indicates good pulmonary blood flow and good cardiac output due to good compressions. If the value of ETCo2 has been below 10 mmHg persistently for 20 minutes after confirmed placement of ETT as well as adequate compressions, it can be used as an indicator for the termination of resuscitation efforts (Assuming you’ve done the whole associated protocol correctly and there are multiple other indicators present before taking a decision). A sudden increase of ETCo2 during CPR may indicate a return of spontaneous circulation where it should prompt the physician to reevaluate the patient but continue adequate ventilation since a patient in ROSC are at high risk of rearrest during the first 10 minutes. The ETCo2 should spike up to somewhere between 35 - 45 mmHg and keep steady with adequate ventilations. A slow decline in ETCo2 after ROSC indicates that CPR might again be needed soon or that administration of vasopressors are needed to increase blood pressure