Endocarditis
Introduction
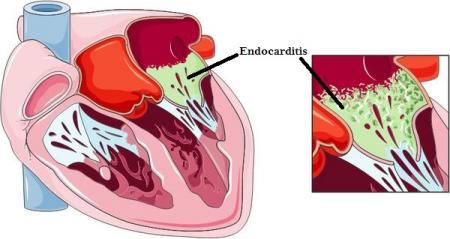
Endocarditis refers to an inflammation of the endocardium (the innermost layer of the heart). It typically involved the heart valves but it may also involve the septum or chordae tendinae. It is often classified as infective or noninfective endocarditis.
Epidemiology
Infective endocarditis is estimated at 15 per 100,000 yearly.
Pathophysiology
Infective endocarditis -
The heart valves are typically protected from infection due to the continuous flow of blood across their smooth surface. However, during infective endocarditis, a damaged heart valve or bacteremia produces conditions that allow for bacteria to form vegetations on the surface of the heart valve. This is further complicated by the fact that heart valves do not contain their own blood supply. The immune system cannot readily reach these bacterial vegetations. Causes typically include rheumatic fever, IV drug use and iatrogenic (heart surgery). Streptoccoci and staphylococcus aureus comprise some 80 to 90% of cases.
Noninfective endocarditis -
Refers to the formation of sterile thrombi on the cardiac valves. The vegetations in and of themselves do not typically cause symptoms but rather from the embolization of the vegetation or if the vegetation later serves as a nidus for infection. Causes include deposition of immune complexes in lupus erythematosus (Libman-Sacks endocarditis) as well as system wide inflammation seen in chronic wasting disease, DIC and metastatic carcinomas (marantic endocarditis).
Signs and Symptoms
Initially, the symptoms are vague and include low grade temperature, easy fatigability, chills and weight loss. Later on, many of the signs are a result of systemic microemboli. These include:
-
Retinal emboli producing round retinal lesions (Roth spots)
-
Cutaneous petechiae
-
Painful subcutaneous nodules on the fingertips (Osler nodes)
-
Hemorrhagic lesions on the palms/soles (Janeway lesions)
-
Splinter nail bed hemorrhages
-
New heart murmur
Emboli can travel to brain causing TIAs and stroke. Emboli to the kidney may cause flank pain. Emboli to the spleen may cause left upper quadrant pain and splenomegaly.
Diagnosis
- Three blood cultures within a 24 hour period
-
Echocardiography
Diagnosis is done according the Duke’s Criteria. Definitive diagnosis is made in the presence of two major criteria, 1 major + 3 minor, or 5 minor criteria.
Major criteria:
-
Typical pathogens in two separate blood cultures
-
Evidence of endocardial involvement by echo
Minor criteria
-
Predisposition: IV drug user or heart surgery
-
Single positive blood culture
-
Fever
-
Vascular phenomena (i.e. petechiae, janeway lesions etc)
- Echocardiographic findings that do not meet major criteria
Treatment and Management
Patients with confirmed endocarditis will require admission and IV antibiotics. Surgery may be required. Definitive antibiotics may vary according to culture data, but initial antibiotic regimens may include:
-
Penicillin G or ampicillin + gentamicin
-
Ampicillin + ceftriaxone
- Vancomycin + gentamicin
References
- Wikipedia: https://en.m.wikipedia.org/wiki/Endocarditis
- Merk Manuals: http://www.merckmanuals.com/home/heart-and-blood-vessel-disorders/endocarditis/infective-endocarditis