Pericarditis
Introduction
Pericarditis refers to inflammation of the pericardium, which is a sac-like tissue that surrounds and supports the heart and great vessels. Pericarditis is a relatively uncommon disorder. It is estimated to affect 3 per 10,000 people per year. The people most commonly affected are males between the ages of 20-50.
Pathophysiology
There are many different causes of pericarditis. The most common cause of pericardium is infection (viral vs bacterial vs fungal). Viral pericarditis is the most common cause of pericarditis in the developed world. Pericarditis can also be seen with malignancies, myocardial infarction (Dressler's Syndrome), autoimmune disorders, uremia (uremic pericarditis), and may be a complication of drug-induced disorders and radiation exposure.
- Common viral etiologies include: coxsackie, echovirus, HIV, mumps, and herpesvirus
- Bacterial etiologies: staphlyococcus, s.pneumoniae, TB.
- Fungal etiologies: histoplasmosis, aspergillus, candida, coccidioides
Medication side effects: Isoniazid, cyclosporine, warfarin, heparin, hydralazine
Signs and Symptoms
The common presentation of pericarditis is typically of sharp, stabbing chest pain that radiates to the neck or back Classically the chest pain worse with deep inspiration and with lying supine. The pain is usually alleviated by sitting upright and leaning forward. Pericarditis may often mimick pulmonary embolism (given the pleuritic nature of the pain) and angina (given radiation to the neck and back). Associated symptoms may include shortness of breath, anxiety, cough, fatigue, and a low grade fever.
Diagnosis
Cardiac exam: On auscultation you may appreciated a friction rub which will be heard best at the left lower sternal border.
Electrocardiogram: The classic finding is diffuse, concave, ST segment elevations in all leads except aVR or V1. You may also see diffuse PR depressions in all leads except aVR
Labs: Cardiac markers such as troponin may be increased. In the case of uremic pericarditis, there may be an increased BUN or creatinine.
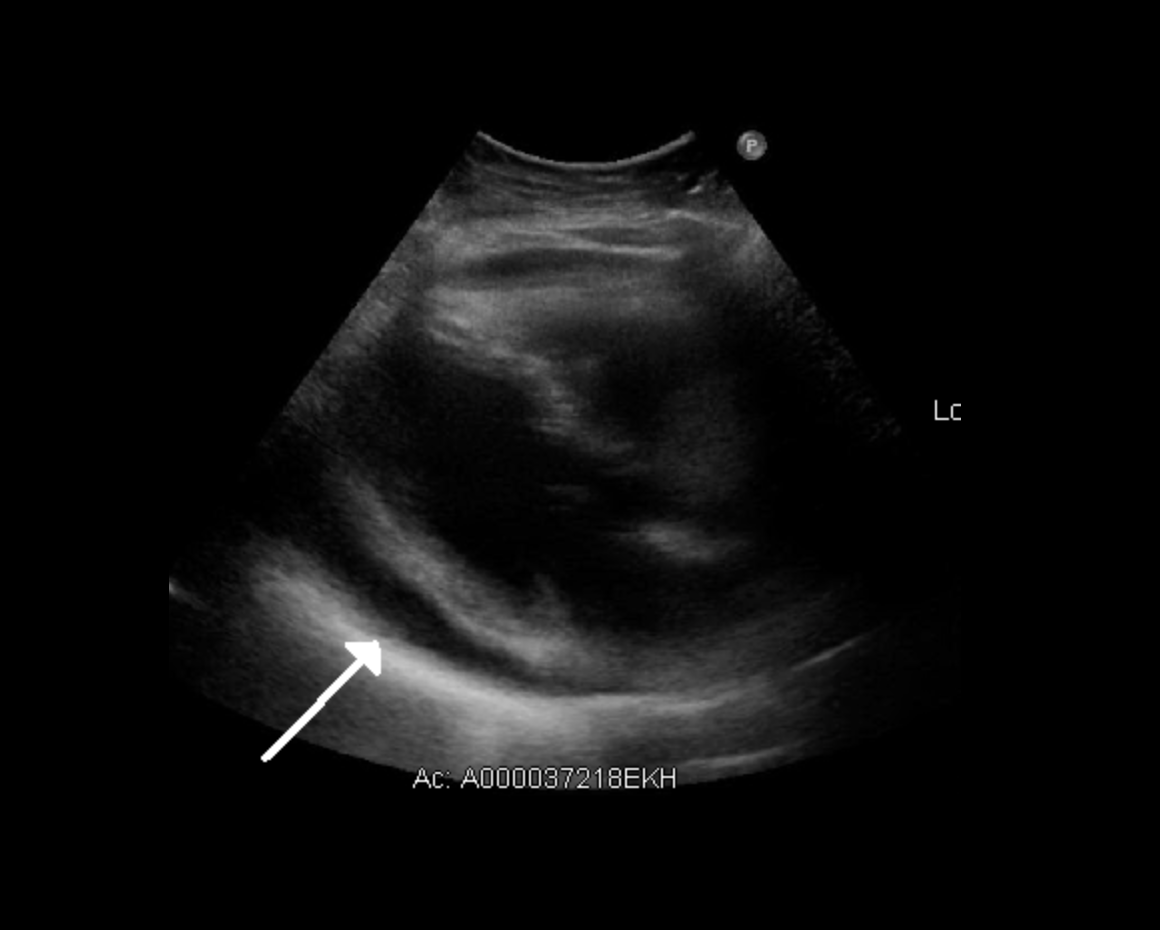
**A common complication of pericarditis is a pericardial effusion which can lead to cardiac tamponade. Always evaluate for pericardial effusion in patients with pericarditis. Signs of cardiac tamponade include abnormal vital signs (hypotension, tachycardia), Becks triad (muffled heart sounds, jugular venous distention, hypotension), and pulsus pardoxus. Obtain and echocardiogram in all patients with pericarditis and obtain an early cardiology consultation in those you suspect have cardiac tamponade physiology.
Treatment and Management
Patients who are stable with a presumed viral etiology without evidence of hemodynamic compromise can be managed as an outpatient. Treatment includes aspirin, NSAIDs, and colchicine.
Patients with evidence of uremic pericarditis, myocarditis or possible hemodynamic compromise (cardiac tamponade) should be admitted for further management.