Intracranial Hemorrhage
Introduction
Intracranial hemorrhages are classified according to the location of the bleed. There are three primary categories. An epidural hematoma refers to a collection of blood between the inner layer of the skull and the dura mater. A subdural hematoma refers to a collection of venous blood between the dura mater and the arachnoid. Finally, a subarachnoid hemorrhage refers to some disruption of the subarachnoid vessels that leads to the presence of blood in the CSF. It is estimated that there are approximately 40,000 to 67,000 cases per year in the United States.
Pathophysiology
Epidural Hematoma
An epidural hematoma is typically associated with an injury to the temporal area of the head which results in laceration of the middle meningeal artery. This leads to a collection of blood between the inner skull and dura mater. Epidural hematomas are rapidly expanding due to the fact that the bleed is arterial and not venous.
Subdural Hematoma
A subdural hematoma results from a tearing of the bridging veins in between the subarachnoid space to the dural venous sinus. This causes blood to pool in between the dura mater and arachnoid. These bleeds tend to collect more slowly as they are under venous pressure.
Subarachnoid Hemorrhage
A subarachnoid hemorrhage may result secondary to trauma or rupture of a cerebral aneursym. Blood will collect in the subarachnoid space.
Signs and Symptoms
An epidural hematoma is classically associated with a head injury, loss of consciousness followed by a ‘lucid interval.’ Oftentimes, the patient may have clear mentation in the ED, before decompensating. A fixed and dilated pupil on the side of the injury is a late finding.
A subdural hematoma classically presents in the elderly or alcoholics (those with some degree of brain atrophy) after a fall or a sudden acceleration-deceleration mechanism. Given the slow nature of the bleed, presentation may be delayed and patients may go diagnosed for up to a week. At this point patients are typically presenting with confusion, lethargy, and increased headaches.
A spontaneous subarachnoid hemorrhage classically occurs as a thunderclap, worst headache of life, event. Patients may complain of diffuse headache, nausea, photophobia, and neck pain/stiffness.
Diagnosis
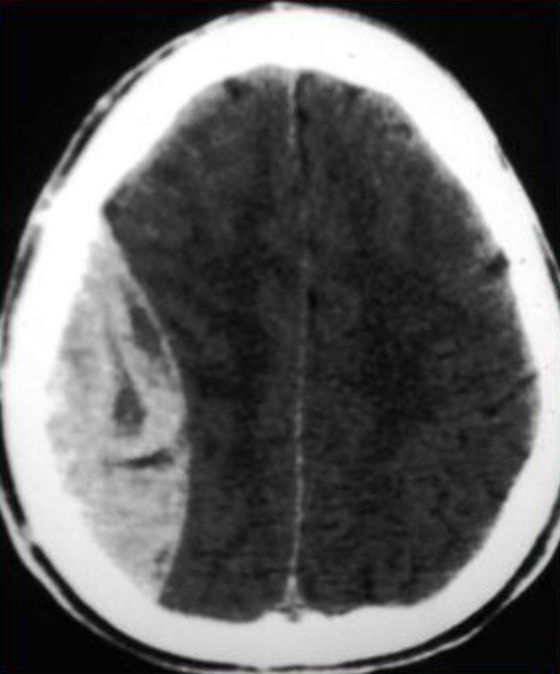
Epidural and subdural hematomas → obtain a STAT non-contrast head CT to evaluate for bleeding. Epidural bleeds tend not to cross suture lines and will show up as a bright white lentiform shaped collection on CT. Subdural hematomas can cross suture lines and will show up as bright white crescent shaped collections on CT.
Subarachnoid hemorrhage → within 6 hours of onset, a head CT is 98% sensitive to capture SAH. If neg head ct and outside of 6 hour window, proceed to a lumbar puncture to definitively rule out blood in the CSF. On lumbar puncture the main finding you are looking for is xanthochromia (yellowish hue to the CSF seconary to red blood cell lysing). You can also look for the percentage decrease of red blood cells between tubes 1 and tube 4. If there is still a significant amount of RBCs in tube 4, this should clue you in to possible SAH.
**Always measure the opening pressure when doing lumbar punctures. An elevated opening pressure is typically not seen with SAH and may help you differentiate between alternative causes of severe onset headache.
Treatment and Management
-
The most important step is to make sure the patient is protecting their airway. Large, rapidly expanding bleeds, or bleeds in the brainstem can cause depression of respiratory effort. Secure the airway with an endotracheal tube if there is any concern that the patient is losing their airway or may potentially lose their airway.
-
Elevate head of bed (HOB) to 30 degrees. After securing the airway HOB elevation is the most crucial initial step to helping decrease intracranial pressure. Intravenous Mannitol is a medication that can be used i the patient is showing signs of increased intracranial pressure (blown pupil) or has signs of increased intracranial pressure on CT (midline shift, herniation).
-
Aim for strict blood pressure control SBP <140mmHg. This cutoff was in part determined by the INTERACT-2 trial which showed that a intese reduction of blood pressure was associated with better neurologic status and quality of life in the long-term. Intravenous Labetalol and the calcium channel blocker Nicardipine are preferred agents for blood pressure control.
-
Obtain a STAT neurosurgery consult for further evaluation and admission to a neurologic intensive care unit (if one is available at your facility). Discuss the possible of starting antiepileptic agents with your neurology / neurosurgery teams.