Vasopressors & Inotropes - The Medications
Norepinephrine
Indications: Septic shock, cardiogenic shock, neurogenic shock
Dose: 0.01 - 3 mcg/kg/min
Adverse Effects: Arrhythmias, bradycardia
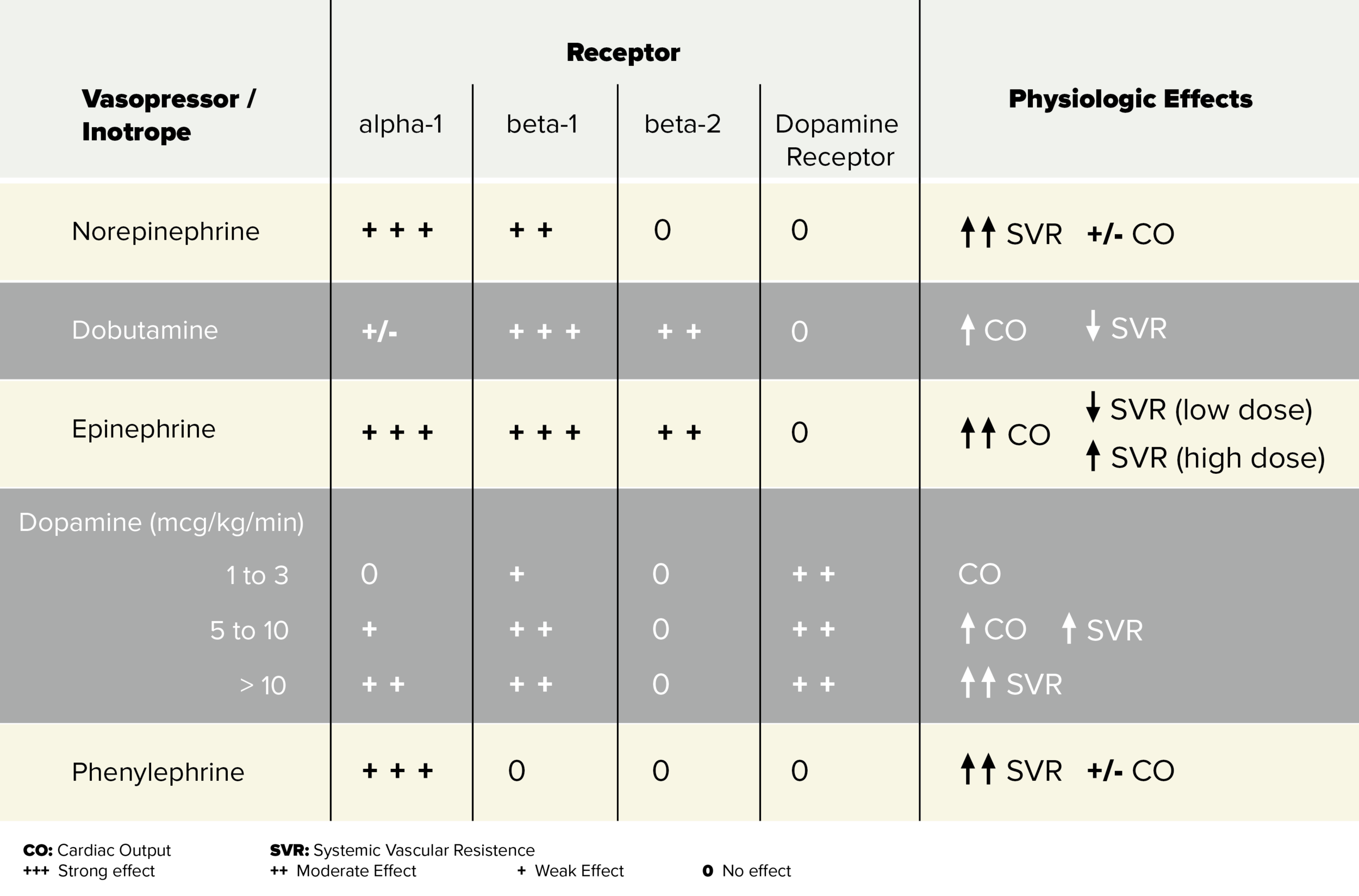
Often used as the first line vasopressor in vasodilatory shock, norepinephrine is one of the most commonly used vasopressors. It is an alpha and beta-1 agonist, although it does have a small effect on beta-2 receptors. By acting on alpha receptors, norepinephrine causes vasoconstriction, increasing mean arterial pressure.
The effects on beta-1 receptors are minimal compared to norepinephrine's effects on alpha-1. It causes an increase in cardiac contractility and as a result, increases stroke volume. Although it does increase heart rate through it's beta-receptor activity, this is cancelled out by the reflex bradycardia caused by its vasoconstrictive effects on our blood vessels. Overall, although the effect on beta-1 receptor is minimal, the effect is an increase in cardiac output.
Dobutamine
Indications: Low cardiac output (e.g. decompensated heart failure, cardiogenic shock, failed septic shock with resuscitation with IV fluids and vasopressors)
Dose: Infusion 2-20 mcg/kg/min (max 40 ug/kg/min)
Adverse Effects: tachycardia, cardiac ischemia, hypotension, arrhythmias
Dobutamine is an inotrope that predominantly acts on beta-1 receptors causing increases in inotropy and chronotropy. This means dobutamine will cause increases in cardiac output with minimal effects on vascular resistance. The effects of dobutamine is also dose dependent. Think of three dose tiers, low, moderate and high doses. The main difference with these dose tiers is the level of activity on the alpha-1 receptor; as doses increase so does the level of activity at the alpha-1 receptor.
At low doses, <5 mcg/kg/min, dobutamine acts on beta-2 and mild effects on alpha-1 receptors. Overall, at low doses, along with increases in inotropy and chronotropy (beta-1 effects), there is a net vasodilatory effect. At moderate doses, 5-15 mcg/kg/min, there is minimal effects on systemic vascular resistance because equal effects at beta-2 and alpha-1 receptors. At high doses, >15 mcg/kg/min, alpha-1 receptor activity predominates, in addition to beta-1 effects on the heart.
Therefore the overall major effect of dobutamine on the body is an increase in cardiac output with minor dose-dependent variations in systemic vascular resistance.
Epinephrine
Indications: Anaphylactic shock, septic shock, cardiogenic shock, neurogenic shock, symptomatic bradycardia, cardiac arrest, bronchospasm
Dose: 0.01-0.1 mcg/kg/min
Adverse Effects: arrhythmias, cardiac ischemia
Epinephrine is the first line vasopressor for cardiac arrest and anaphylaxis. Epinephrine acts mostly on beta-1 receptors, however there is some beta-2 activity and also dose dependent alpha-1 activity. At low doses (<10 mcg/kg/min), epinephrine predominantly acts upon beta-1 receptors causing increases in cardiac contractility and heart rate, therefore an overall increase in cardiac output. At these low doses epinephrine has less prominent effects on beta-2 receptors causing vasodilation and at alpha-1 receptors causing vasoconstriction. Because of mild effects on both beta-2 and alpha receptors, changes in blood pressure is variable or unchanged.
At higher doses (>10 mcg/kg/min), epinephrine's effects on alpha receptors predominates, thus causing increases in systemic vascular resistance through vasoconstriction. It still has effects on beta-1 receptors and at these higher doses, you will also see increases in cardiac output.
Dopamine
Indications: symptomatic bradycardia, septic shock, cardiogenic shock, neurogenic shock
Dose: Infusion 2-20 mcg/kg/min
Adverse effects: arrhythmias, cardiac ischemia
Dopamine acts on dopamine receptors with dose dependent physiologic effects. You can think of these doses as low, intermediate and high doses of dopamine. At low doses of 1 to 2 mcg/kg/min, dopamine acts predominantly on dopamine-1 receptors in the renal, mesenteric, cerebral, and coronary beds, resulting in selective vasodilation.
At 5 to 10 mcg/kg/min, dopamine also stimulates beta-1 receptors. Therefore at these doses, dopamine causes increases in heart rate and stroke volume leading to increases in cardiac output.
At doses >10 mcg/kg/min, the predominant effect of dopamine is to stimulate alpha receptors. This causes an increase is systemic vascular resistance.
Phenylephrine
Indications: medication or vagal induced hypotension (e.g. post-intubation), septic shock
Dose: Infusion 0.4 - 9.1 mcg/kg/min, Bolus 0.1-0.5 mg IV every 10-15 min
Adverse Effects: Reflex bradycardia, peripheral vasoconstriction causing ischemia
Phenylephrine as a pure alpha-adrenergic agonist. Therefore it will cause vasoconstriction and thus increases in systemic vascular resistance. You will often see phenylephrine in pre-made syringes to be used peripherally. Thus access to this "push-dose" peripheral pressor can be an attractive alternative when central access is not immediately obtained or necessary, such as in post-intubation hypotension.
Isoproterenol
Indications: Symptomatic bradycardia, polymorphic ventricular tachycardia, Brugada Syndrome
Dose: Infusion: 0.01 - 0.05 mcg/kg/min
Adverse Effects: Arrhythmias, cardiac ischemia
Isoproterenol is a beta-1 and beta-2 agonist. Activation at these receptors causes increased heart rate and contractility. Though it's beta-2 activity it causes smooth muscle vasocontriction in blood vessels resulting in decreases in systemic vascular resistance. Clinically, isoproterenol is rarely used; it is used as a second-line agent for symptomatic bradycardia and torsades de pointes with bradycardia.
Other Vasopressors
VASOPRESSIN
Indications: refractory septic shock, cardiac arrest
Dose: Infusion: 0.01 -0.1 units/min
Adverse Effects: Arrhythmias, cardiac ischemia, mesentery ischemia
Vasopressin is a non-catecholamine peptide, aka antidiuretic hormone. It is often used as a second line agent in refractory vasodilatory shock and is also commonly used in conjuncture with other vasopressors and inotropes (e.g. norepinephrine, epinephrine) when an adequate mean arterial pressure cannot be maintained with one vasopressor alone. The use of vasopressin alone in shock is not recommended. The main physiologic effect of vasopressin is in increasing blood pressure. It acts on vasopressin receptors (V1 and V2 receptors) which are found on vascular smooth muscles walls and also in the the collecting system of the kidneys. Action on these vascular smooth muscles causes vasocontriction and increases in systemic vascular resistance. Vasopressin has minimal effects on cardiac output.
MILRINONE
Milrinone is a phosphodiesterase inhibitor mostly used in decompensated heart failure and in low-output cardiogenic shock. It acts by inhibiting the degradation of intracellular cAMP therefore increasing myocardial contractility. Because of its mechanism of action, it also causes systemic vasodilation. Milrinone is mostly used as a second line agent in decompensated heart failure or when there is chronic use of adrenergic agents such as in chronic heart failure patients.
