Emergency Pericardiocentesis
Introduction
Pericardial effusion and cardiac tamponade are potentially life threatening clinical presentations which can lead to death if not immediately treated. The effusion around the heart is typically evaculated by performing a pericardiocentesis. Some form of this procedure has been described since the mid-1600s, but still remains the standard approach for evacuating life threatening effusions. Advances in medical procedure have lead to the use of ultrasonography the help visualize the pericardial effusion to be drained. Although this procedure should be performed by a knowledable practitioner in the emergent procedure even in the abscence of bedside ultrasound
Cardiac Tamponade
Some findings of cardiac tamponade include:
- Beck's Triad: lower blood pressure, increased JVP, and muffled heart sounds
- although this is only present in a minority of cases. [1]
- EKG: Sinus Tachycardia or electrical alternans
- Ultrasound: showing a pericardial effusion and right ventricular collapse
For more information on cardiac tamponade.
Indications & Contraindications
Indications
Generally, a patient who has a pericardial effusion with unstable vitals signs is an indication for a pericardiocentesis
Contraindications
- Patient's who have stable vital signs
Relative contraindications
- Traumatic pericardial effusion with unstable vital signs
- Patient meets indications for emergent thoracotomy
- Rapid reaccumulation of blood within pericardium
- Myocardial rupture
- Aortic dissection
- Severe bleeding disorder
Equipment
Before proceeding with the procedure it is a recommended that you have an EKG for the patient, you place the patinet on a cardiac montir and defibrillation pads.
- 18-Gauge spinal needle
- three-way stopcock
- 20cc+ syringe
Option (especially if doing a emergent procedure):
- Antibacterial skin cleanser
Procedure
1. Visualize:
using a bedside ultrasound identify the pericardial effusion from a subxiphoid approach. This will also be your guide to where you will insert your needle.
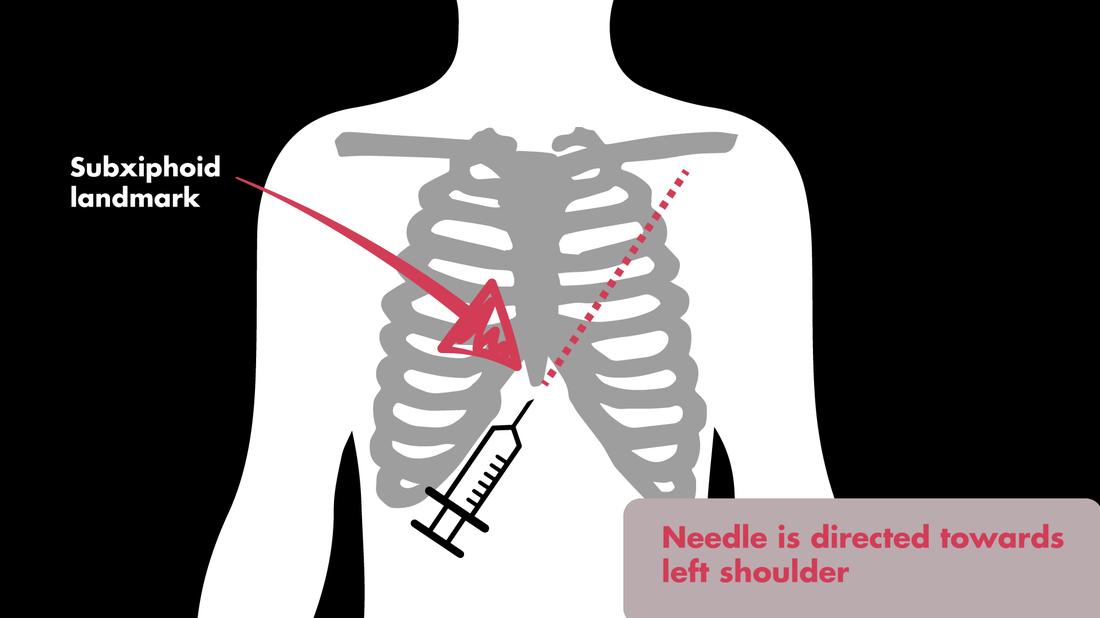
2. Palpate:
for your landmarks specifically noting the location of the subxiphoid area.
3. Prepare:
if you have time, clean the patient’s skin with antibacterial cleanser, drape the surround area and administer local anesthesia
4. Insert:
from a subxiphoid approach, insert and advance your spinal needle, aiming towards the patient’s left shoulder. While advancing your needle continuously apply negative pressure until you receive a flash of pericardial fluid or can visualize your needle in the pericardial space on ultrasound. Continue evacuating fluid until the patient’s vital signs normalize or when you cannot remove any more fluid from the pericardial space.